Frozen Shoulder: Does it Really Thaw?
Frozen shoulder is a very painful shoulder condition, yet most people forego getting treatment. They simply try and “wait it out.” It has always shocked me how long patients tolerate the pain of frozen shoulder before getting treatment. But once they start the process of physical therapy, every single patient says: “Why didn’t I do this sooner?” That’s MY question. Why aren’t you doing it sooner? What makes people hesitant to get treatment for frozen shoulder? It all started back in 1934…
 Frozen shoulder (also known as adhesive capsulitis) was first named by Ernest Amory Codman in 1934. Codman was a medical doctor in Boston, now famously known for the Codman’s Exercises (see picture to right). At that time, he wrote that frozen shoulder is “difficult to define and difficult to treat.” This continues to be the consensus in the medial profession. However, I have found with a little patience and the right exercises, frozen shoulder is not that difficult to treat.
Frozen shoulder (also known as adhesive capsulitis) was first named by Ernest Amory Codman in 1934. Codman was a medical doctor in Boston, now famously known for the Codman’s Exercises (see picture to right). At that time, he wrote that frozen shoulder is “difficult to define and difficult to treat.” This continues to be the consensus in the medial profession. However, I have found with a little patience and the right exercises, frozen shoulder is not that difficult to treat.
After Codman first described frozen shoulder, the medical community adopted the theory that frozen shoulder was caused by inflammation. And, like other inflammatory events in the body, it naturally progressed through specific phases of recovery.
- Phase I – Inflammatory Response: Blood flow increases to the injured area, bringing in new cells and collagen (the protein stuff that builds healthy tissue) to initiate healing. Damaged cells are taken away from the area. This phase usually last 3-5 days.
- Phase II – Repair and Regeneration: Collagen begins to form into disorganized bundles, which create weak and fragile scar tissue. This phase usually last 2-10 weeks.
- Phase III – Remodeling and Maturation: Collagen begins to organize itself into strong bundles for healthy tissue. This phase can last for months.
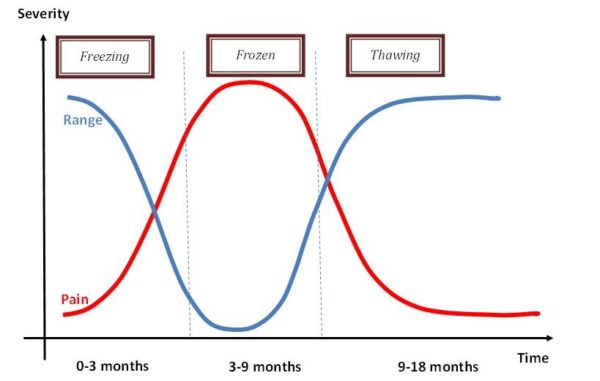
In 1975, Reeves hypothesized that frozen shoulder went through 3 distinct stages: pain, stiffness and thaw. He concluded that the condition was self-limiting and would resolve itself on its own. Well, guess what. There is absolutely no research that finds this to be true. Seriously. Zero. Zilch. Nada. Although frozen shoulder MAY begin because of irritation and inflammation to the area, the research does not support the thaw theory. And, clinically, I have never seen a frozen shoulder “just works itself out.”
Below are the parameters that Reeves found to be true…that is if you skip treatment!
- Pain Duration – 10-36 weeks. 36 weeks!!?? Can you imagine being in pain for 9 months?
- Shoulder Stiffness Duration – 4-12 months. One year of not being able to move your shoulder?
- Recovery Time Frame or THAW – 5-26 months. Seriously…2 years!!
- ***none of the patients ever made a full recovery!
There is absolutely no reason to be in pain with this condition. It’s very treatable with physical therapy.
Here’s a graph I found on the web that demonstrates the popular thought behind frozen shoulder…but now you know it doesn’t really thaw.
Shoulder Review
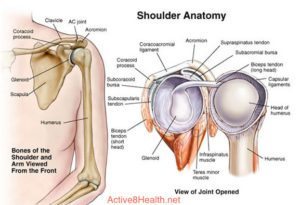 The shoulder complex is a combination of the scapula (shoulder blade), clavicle (collar bone) and humerus (arm). Each of these bones move to create all of the motion at the shoulder. Frozen shoulder specifically affects how the humerus moves on the scapula or the glenohumeral joint.
The shoulder complex is a combination of the scapula (shoulder blade), clavicle (collar bone) and humerus (arm). Each of these bones move to create all of the motion at the shoulder. Frozen shoulder specifically affects how the humerus moves on the scapula or the glenohumeral joint.
The glenohumeral joint is a ball and socket joint. It is very shallow (only a small portion of the humerus communicates with the scapula) and relies on ligaments, the capsule and muscles to keep it moving and stable. This combination of the ball and socket joint and it being shallow, allows the shoulder to move into incredible ranges of motion. We can move our arm up our back, overhead, out to the side and even use it to throw a ball.
To truly understand the awesome motion at the shoulder, think of your hip. It is also a ball and socket joint with ligaments, a capsule and muscles. BUT, it’s not shallow. The head of the thigh bone sits deep into the pelvic socket. Considering all of the motion of the shoulder, can you imagine trying to move your leg up your back? Me neither.
What is Frozen Shoulder?
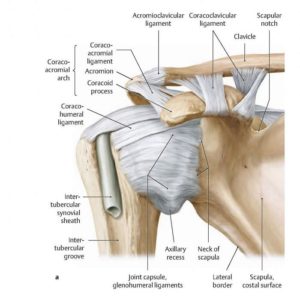 Frozen shoulder is a condition of the glenohumeral joint, specifically the anterior (front) capsule. The capsule becomes dense and thick, especially at the rotator interval (the area between the acromion and coracohumeral ligament) and axillary recess (the bottom portion of the capsule). In addition, the coracohumeral ligament becomes super thick and extra fibroblasts (cells that make collagen) and synovitis (inflammation of the fluid within the joint) are present. Basically, your shoulder is a hot mess. And, really painful. Without treatment, you lose the ability to reach above 90 degrees and the pain becomes more and more intense, especially at night.
Frozen shoulder is a condition of the glenohumeral joint, specifically the anterior (front) capsule. The capsule becomes dense and thick, especially at the rotator interval (the area between the acromion and coracohumeral ligament) and axillary recess (the bottom portion of the capsule). In addition, the coracohumeral ligament becomes super thick and extra fibroblasts (cells that make collagen) and synovitis (inflammation of the fluid within the joint) are present. Basically, your shoulder is a hot mess. And, really painful. Without treatment, you lose the ability to reach above 90 degrees and the pain becomes more and more intense, especially at night.
Symptoms of Frozen Shoulder
- Stiffness of the shoulder with functional tasks
- Shoulder pain with movement, at night and at rest
- Difficulty reaching behind your back, overhead and out to the side
Question and Thought…
 Have you ever been so thirsty or taken a narcotic pain pill and your mouth is really dry? Your saliva feels thick and so you just keep your mouth closed to avoid the sensation. Because, when you open your mouth your lips start to stick together? And how do we resolve it? We drink water.
Have you ever been so thirsty or taken a narcotic pain pill and your mouth is really dry? Your saliva feels thick and so you just keep your mouth closed to avoid the sensation. Because, when you open your mouth your lips start to stick together? And how do we resolve it? We drink water.
This is basically what is happening with frozen shoulder. The shoulder capsule starts to thicken, we move it less and less until it becomes one sticky, stiff joint. How do we resolve it? We give it fluid. In a healthy joint, synovial fluid sits inside the joint to provide lubrication and nutrition. The synovial fluid stays healthy and “fresh” by movement.
What Causes Frozen Shoulder?
Well…that’s the kicker! We really don’t know what causes insidious frozen shoulder (insidious onset: it occurs so gradually and subtly that you have no idea it’s happening). So, yes, it can actually just show up one day. There are some correlations with diabetics and menopausal women (hormone related), but the research is still inconclusive. Clinically, I have treated women 45-60 with frozen shoulder more than any other population. So, there’s that.
We do know that lack of motion leads to frozen shoulder. Lack of motion can happen after a painful sprain or shoulder surgery as the patient likes to protect the arm and hold it at their side. This is why safely moving the shoulder after an injury or surgery is imperative!
I always tell my patients, the worse thing you can do for frozen shoulder is not move it!
What is the Treatment for Frozen Shoulder?
You guessed it, MOVEMENT. If you’ve ever had frozen shoulder, you know that moving your arm into painful zones is the LAST thing you want to do. But, movement is the magic power behind treating this condition. The movement does not have to be overly aggressive, just effective. After 3-4 treatments, the pain is usually significantly less, shoulder motion is improved and you sleep better at night. That last part is worth every bit of therapy!
Case Study

A very active 63-year-old woman hurt her left shoulder in November of 2015. For months, she continued to “work through” the pain, even exercising through the discomfort. She was doing push-ups and weight lifting with 8/10 pain that worsened at night. In February 2016, 4 months later and 4 months after she was referred to me, she came to the clinic.
She had strained her left shoulder in November, but over time she stopped moving her shoulder into certain zones. In those 4 months, she developed frozen shoulder that was making her pop ibuprofen like candy. But, after 3 treatments her pain was much less (3/10) and she wasn’t taking ibuprofen anymore. After 4 treatments, her pain at night was gone. After 2 months, she reported 90% improvement. I saw her a total of 9 visits in 4 months.
What was her treatment plan? Manual therapy for joint mobility and soft tissue manipulation, ROM (range of motion), scapula/core training and rotator cuff exercises. Yes, that’s it
Thank you for reading! If you enjoyed this post and found it helpful, please share so others can learn too.
© 2017 & Beyond. ALL BLOG CONTENT at duncansportspt.com by Lori Duncan PT
ABOUT THE AUTHOR
 Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
References
![]()
Reeves B. The natural history of the frozen shoulder syndrome. Scand J Rheumatol. 1975;4(4):193-6.
Ryan V, Brown, H, Minns Lowe CJ, Lewis, JS. The pathophysiology associated with primary (idiopathic) frozen shoulder: a systematic review. BMC Musculoskelet Disord. 2016;17:340.
Wong CK, Levine WH, Deo K, et al (in press). Natural history of frozen shoulder: fact or fiction? A systematic review. Physiotherapy. June 2016.

I know your therapy works as I am proof of that fact! I was facing surgery for my shoulder and after a number of physical therapy sessions I now have more range of motion than I had even before my shoulder issue. and I have not had any surgery!
Thanks Bob! It’s always such a pleasure to work with you. See you soon!
I had surgery for rotator cuff tear and frozen shoulder in July ( 4 screws and sutures) had manipulation surgery 3 wks ago but doesn’t look like they moved it in all directions. I still cant move my shoulder when they lift my arm up the ball doesn’t move, the shoulder is lifting with my back . the ball is stuck and my back is taking all the strain my scapula sticks out my back when they lift my arm. My 2nd opinion says I have to do therapy for 2 years. My therapist has been doing aggressive therapy for 4 wks and now he thinks it ripped again. He said I have to do it on my own now and then see the doctor Imagine liftin your arm up when the balls not moving so the muscles are stretching around the ball. In July they should of done a capsule release but didn’t. now I have to suffer. I don’t know what to do.
Hi Lise,
Sorry I missed this. 2 years of therapy is ridiculous. 6 months…maybe. I would get an MRI to see if it is truly torn. If not, get a good therapist that will be PROgressive, not aggressive. Very different approaches. Hope that helps!