IT Band Syndrome: Look for Your Glutes NOT the Foam Roller!
Raise your hand if you have had sharp pain on the outside of your knee or leg, maybe after running or hiking? Keep raising your hand if someone said: “Oh, just roll on the foam roller and you’ll be good to go!” I feel a lot of hands up right now.
I wish it was that simple. I do have some of my patients use the foam roller for myofascial release, but it is a teeny-tiny portion of the exercises prescribed to truly rehabilitate IT band syndrome. Is the foam roll helpful? Sure. But, excessively rolling on a piece of styrofoam tubing is not going to actually fix the injury or yield long-term results.
And, this is not just a runner’s injury, it’s a movement injury. If you walk, cycle, hike or climb stairs, this is a syndrome that could creep into your life one day. But, it doesn’t have to. Hip and lower extremity biomechanic training is the best, most-researched route to tackle this injury.
What is IT band syndrome?
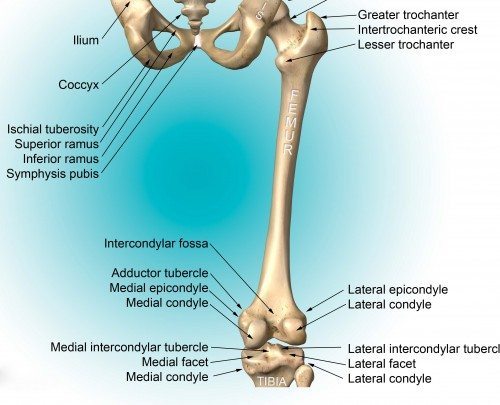
IT band syndrome is sharp lateral (outside) knee or thigh pain that is commonly exacerbated by repetitive activity such as: running, cycling or walking. “IT” stands for iliotibial because of its vast expansion from the ilium (hip) to the tibia (lower leg). This syndrome is usually caused by tightness and/or irritation of the IT band. The big question: why is the IT band tight and irritated?
Answer: THE GLUTES ARE WEAK. This will make more sense in a bit.
In the past, this syndrome has been termed “IT band friction syndrome.” The thought was that the IT band was gliding across the femoral lateral epicondyle (bony bump on femur) at approximately 30° of knee flexion. When it became tight (from repetitive movement), the band would “friction” and become irritated over the lateral epicondyle. This friction would result in pain. However, new research is indicating something else may be happening.
Anatomy Associated with IT band Syndrome
Definitions
- Ilium: the hip bone
- Femur: the long thigh bone
- Tibia: the larger lower leg or shin bone
- LFE: lateral femoral epicondyle: a site of attachment and pain of the IT band
The iliotibial band is a thickened part of the fascia lata (deep connective tissue of the thigh) that spans from the hip to the knee. The band anchors from the ilium and travels down the leg to insert around the LFE and at Gerdy’s tubercle on the tibia. The gluteus maximus has a significant insertion into the IT band and current research suggests that the IT band could be considered a tendon of the gluteus maximus. Histology research (the study of tissues) supports this theory: the tissue from the hip to the LFE is similar to tendon and the tissue from the LFE to Gerdy’s tubercle is similar to ligament. The tensor fascia lata (TFL), quadriceps and hamstrings (front and back thigh muscles) also communicate with the IT band.

IT Band Anatomy: Lateral and Anterior View. Area of pain indicates the location of the LFE and the usual site of sharp pain.
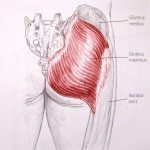
Gluteus Maximus. This muscle is the usual culprit of IT band syndrome. It makes sense, though. Look at how massive this muscle is compared to the other hip muscles. The picture shows how the gluteus maximus dominates most of the IT band. So you can see the importance of having a gluteus maximus that works. The reason most people get IT band syndrome is because they are dominant in their anterior muscles (TFL and quadriceps) and have do not have a gluteus maximus to balance everything out.
Gluteus Medius. This is the main stabilizer of the pelvis and super important when the foot is on the ground. If the pelvis isn’t stable, nothing really works right. RECRUIT THE GLUTES!
What is the role of the IT Band?
Along with serving as an attachment site for the hip and thigh muscles, it resists the varus force at the knee (well, the hip too), but for now we will focus at the knee. Ok, the varus what?
Stand up and look down at your right knee. Now, step back with your left leg. Your right knee is exposed in front. Imagine a ball or child hitting the inside of your knee. First, ouch. Second, this is a varus force (medial force) against your knee and the IT band resists this force to protect the knee. Of course, our daily routine does not fear a blunt force on the inside of the leg, so how is the IT band continually resisting varus force?
Christopher Powers, PT, PhD has done some very cool research about ground reaction force vectors with walking and running. His research shows that when our foot strikes the ground, there is a varus force vector that consistently travels to the hip. This makes sense anatomically. Think of where all of our big, bulky hip and leg muscles are…on the outside, not the inside. Where is the thick IT band? Again, on the outside of the leg. These bigger muscles and thick fascia help resist the medial force vector (pain-free, mind you) when the pelvic mechanics are normal (figure A). However, if you change the pelvic position (figure B and C), the force vector changes and soft tissue stress or injury is a likely result.
A. Shows the normal force vector with a stable pelvis. Gluteus maximus, medius, core stabilizers and IT band are happy and healthy.
B. Shows the force vector moving farther away from the knee, so the IT band and outside structures have to work extra hard to resist the force vector. It also demonstrates what the pelvis does with gluteus medius weakness.
C. Shows the vector moving to the opposite side of the knee, resulting in medial knee pain and ACL vulnerability. It demonstrates a compensation of gluteus medius weakness. The pelvis looks level, but what you don’t see is the trunk bending over that pelvis, and that changes the vector.
So, if it’s not about the foam roller…what is it about? (in order of importance)
- Exercise that emphasizes pelvic stabilization and strength (core, glutes, hip rotators)
- Neuromuscular education that teaches the TFL and quadriceps muscles to chill out because they are usually dominant and dysfunctional
- Manual therapy to release myofascial restrictions along the IT band anatomy
- Flexibility to the hip and lower extremity muscles
- Ice massage to the IT band if it is inflamed. (If it is tender to the touch, it’s likely inflamed. DON’T FOAM ROLL during this phase.)
If you must foam roll, just a note: avoid rolling over the bony landmarks. It can cause bursitis at the hip and bone irritation at the knee. Stay on the main track between the upper thigh and knee.
New research
Researchers (Fairclough, et al) are challenging the idea of the IT band moving across the femoral lateral epicondyle. Although research does show posterior (backward) movement of some IT band fibers with knee flexion, researchers are now asking this question: is the band actually moving or are the fibers being pulled posteriorly because of mechanics and tightness? The new thought is that the IT band, especially if dysfunctional and tight, is compressing a highly innervated fatty tissue between the band and bone. Highly innervated= lots of opportunity for pain. Continued research is in the works to test this new theory.
Final thoughts:
Whether the syndrome is friction, compression or tightness, research indicates that hip mechanics and strength are the main key to resolving this issue. Clinically, I have had excellent results with patients who present with IT band syndrome. As long as patients do their homework and find their glutes and core, the rest takes care of itself.
© 2014 and Beyond. ALL BLOG CONTENT at duncansportspt.com by Lori Duncan PT
BLOG TALK PODCAST
Blog Talk – IT Band Syndrome
ABOUT THE AUTHOR
 Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
References:
Fairclough J, Hayashi K, Toumi H, et al. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. J Anat 2006; 208:309–316
Fairclough J, Hayashi K, Toumi H, et al. Is iliotibial brand syndrome really a friction syndrome? J Sci Med Sport 2007; 10:74–76
Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, Sahrmann SA. Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med. 2000;10:169–175
Jelsing E, Finnoff J, Chevill A, Levy B, Smith J. Sonographic evaluation of the iliotibial band at the lateral femoral epicondyle: does the iliotibial band move? J Ultrasound Med. 2013;32:1199-1206.
Powers, C.The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40(2):42-51.

Great post. Interesting finding out about the new research
Thanks for reading! It is interesting research.
Interesting info. The new research is intriguing. Thanks for sharing!
Thanks for reading Jennifer! I love new research.
For about 9 months I have had a pain in my glutes, quads and ITB band also my lower back I have managed to keep on running and racing also lots of stretching and tennis ball plus foam rolling, and of course it hasn’t improved. I have been told I have some wear and tear on my left hip, nothing too bad though. I have also been told not to do any side movements. After my last race which went very well I seized up and have now injured with very tight glutes, after just reading your post on periformer I am now putting your two main exercises into my programme also taking out bridge and no more foam roller thank you so much as every time I stretched I was getting tighter I just want to get back to running, any other advice would be grateful
Hi Ann,
Happy to hear you are trying to get those “good glutes” activated. Instead of static stretching (holding the stretch for a while) I would try some dynamic movements to create mobility in your joints and tissue. See if that makes a difference too.