Back Pain: Disc Herniations
Slip a disc? Back “go out”? Unfortunately, back pain is very common and ~60-80% of us will deal with it at some point. Disc Herniations are one of the most common causes of back pain. Why? Because our body mechanics, core stability, posture and overall movement patterns are not what they used to be. We are sitters who then participate in very intense exercise. OR, we are sitters who sit a little more while watching TV at home. Moderate exercise is not the fad these days.
But one day you go to put on your pants or teach your kid how to ride a bike without training wheels and your back “goes out.” These simple activities have now caused extreme pain. For clarification, nothing slips or goes out in your back. But, the initial pain does feel like something might be broken back there. The good news? Most disc herniations will heal on their own without any surgical intervention.
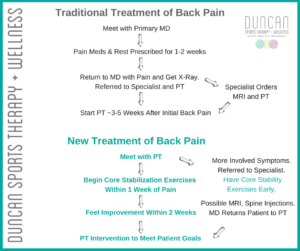
The traditional system of treating back pain is long, costly and doesn’t get you to PT until WEEKS after your symptoms begin. The new system focuses on active recovery, not pain pills and rest.
Research proves over and over again that in the short-term, a microdisectomy can help with symptoms. In the long-term (1 year+ later) there is absolutely no difference in the result of people who had surgery or didn’t have surgery. I’m not sure about you, but if the pain was tolerable, I would much rather work on core stabilization than have a surgical knife in my back.
What is a Disc Herniation?
Spine Review
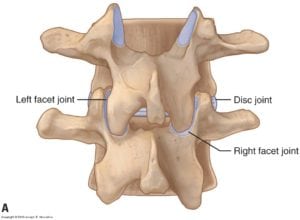 Our spine is made of vertebral bodies, facet joints and intervertebral discs.
Our spine is made of vertebral bodies, facet joints and intervertebral discs.
The vertebrae give structure and stability to the spine to protect the the spinal cord and nerves. The facets joints (similar to a gliding hinge) guide movement in the spine. They determine the direction of the spine: forward, back, to the side or to rotate.
The discs create space for the nerves to run out, but they also allow for movement at each level. They also play a role in force attenuation, dispersing the forces equally throughout each segment.
So, the facets and discs allow for healthy movement of our spine.
Disc Anatomy Review
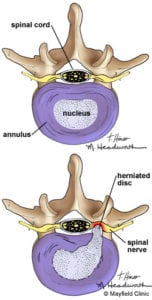
The disc is made of the nucleus (left picture) and outside annulus fibrosus. The inside nucleus is a gel-like substance that allows for all of the good spinal movement. The outside annulus is made of rings that give structure to the disc so we don’t have gooey gel just running all over.
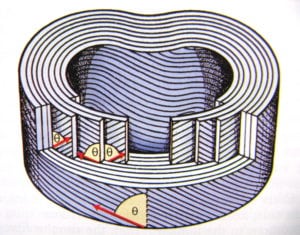 These annular rings are connective tissue and arranged in 10-12 layers of alternating diagonal patterns (//// \\\\ ///// \\\\\). This alternating pattern allows for a pretty tough ring. (right picture)
These annular rings are connective tissue and arranged in 10-12 layers of alternating diagonal patterns (//// \\\\ ///// \\\\\). This alternating pattern allows for a pretty tough ring. (right picture)
Disc herniations can occur with the annular rings partially intact or with a full disruption.
When a disc herniates, it presses out into the space where the nerve runs. If the herniation is big enough, it will start to press on the nerve. This is when we feel pain.
Note: Research states that ~25-35% of us are walking around with a disc herniation. But, the herniation is not large enough to press on any nerve structures. It’s just poking it’s little head outside the edge of the vertebrae. (Like a turtle peeping it’s head out of its shell). But, because the disc herniation is not touching any nerve structures, we have absolutely no clue!
***P.S. This doesn’t mean to run to your local MRI shop and spend $1000 to find out if you have one. Just note, disc herniations can be common, but not problematic. It is the reason everyone should really work on core stabilization though!
4 Stages of Disc Herniation
A disc herniation has 4 stages. Each stage is a little more serious than the previous one.
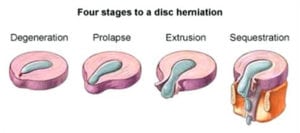 Degeneration – the herniation some of us are walking around with and don’t know about. Usually non-painful.
Degeneration – the herniation some of us are walking around with and don’t know about. Usually non-painful.- Prolapse – this stage is usually when the edge of the disc starts to press on the nerve. Now we feel pain.
- Extrusion – the outside annular ring is broken and disc “gel” can ooze out. Now our pain increases.
- Sequestration – the disc has now “exploded” and stuff is oozing everywhere.
- You need to choose the letters MD over PT at this point
Common Risk Factors for Disc Herniations
- Being Male. Men are twice as likely to get a disc herniation.
- Middle-Aged. Herniations are most common between 30-50 years of age.
- Overweight
- Smoker
- Sedentary Lifestyle
Common Causes of Disc Herniations
 Lift and Twist Movements: shoveling snow, lifting children from the floor or car, moving furniture, poor chop/lift exercise at the gym. You should NEVER Lift and Twist.
Lift and Twist Movements: shoveling snow, lifting children from the floor or car, moving furniture, poor chop/lift exercise at the gym. You should NEVER Lift and Twist.
Here’s a link to previous blog that talks about this specifically: NEVER Lift & Twist
- Extreme Forward Bending Moments (without core control): putting on shoes while standing, teaching a kid to ride a bike, sitting with slouched posture.
- Any movement that causes a load on the body while your core is asleep.
Symptoms of Disc Herniations
Honestly, these can be all over the place. Some people have leg pain, some don’t. Some people have back pain, some don’t. What I’ve realized over the years, most people have some sort of glute pain. Most people have most pain with sitting. Almost all of them say “my back went out again.”
Common Signs: Choose PT
- Back and/or glute Pain- with or without leg pain
- Possible tingling/numbness in the leg or foot
- Pain with sitting, sit to stand and rolling over in bed
- Difficulty standing up straight in the acute phase
- Weak or vulnerable sensation in the back
- Ankle or toe weakness noted – nothing significant
More Involved Signs: Choose MD
- Leg that wants to “give way” or no longer support yourself – can be random
- Significant motor weakness: drop foot, tripping on foot
Emergency Signs – Choose MD – Seriously, go to the ER right now!
- Change in bowel or bladder
What Are Safe Exercises?
Core stability exercises are the most important intervention for disc herniations and any back pain for that matter. The deep abdominals and back stabilizers get sleepy with back pain. So, we have to wake them up!
Note: These exercises are not meant to replace an evaluation with your physical therapist.
Until you can get in with your PT, these are safe on the spine. It’s imperative to start on core stability right away. The position of being on your hands and knees is usually the most tolerable and lying on your side. Here is a video link demonstrating a few safe exercises:
Back Pain: Safe Exercises for Core Stability
Clinical Case Studies
Case Study #1 – A Father Who Was Teaching His Kid to Ride a Bike
 A 45 y.o. father and avid exerciser was helping his 5 year old learn to ride a bike without training wheels. His back was rounded over and he was running. After a few minutes, he said he suddenly went down on his knees in extreme pain.
A 45 y.o. father and avid exerciser was helping his 5 year old learn to ride a bike without training wheels. His back was rounded over and he was running. After a few minutes, he said he suddenly went down on his knees in extreme pain.
His posture was immediately affected and had 8+/10 pain with walking, standing, sleeping and just being alive. He was pretty miserable. He did not state any pain into his leg, just left-sided back and glute pain. No loss of foot or ankle strength and mild numbness down his leg.
After 2 weeks of PT exercises for core stability, walking and upright easy cycling, he reported 50% improvement.
Six weeks after his initial injury, he reported 80-85% improvement. His back was stiff in the morning, but he no longer had pain and could sleep through the night. And, he had returned to the gym to weight lift, cycle and swim.
He did report he was doing his PT everyday and it was very helpful.
Do I know for sure he herniated his disc? No. My clinical experience thinks it’s highly likely. But, there was no reason to send him for an expensive MRI because he was improving. And, he represents the majority of all of us. Most of our disc herniations will heal naturally. They just require some patience and good PT intervention.
Case Study #2 – A Triathlete With a Really Messy Disc
Conservative treatment will never cause damage, but sometimes it’s not enough. Here’s a story of when surgery is the right intervention…
A 40 y.o. triathlete presented with left hip and hamstring pain. She had symptoms for ~6 months. She was training for the Boulder Half Ironman and was DETERMINED to finish it. However, running had become very painful in her hamstring. And, sitting was terrible. Her initial symptoms pointed to a hamstring strain.
After 4 weeks, she was feeling significantly better and back to running 5 miles.
3 weeks later, her pain returned. A visit to the ortho MD showed no disc space at L5/S1. She was referred to a physiatrist for an MRI which found a herniation at L5/S1. It wasn’t large enough to cause surgical concern at this point.
She tried 2 spinal injections and returned to training for her Half Ironman. With pain, she was able to finish her race.
8 months after beginning PT, she had a microdiscectomy (partial removal of the disc hitting the nerve) at L5/S1. Her pain resolved, and she returned to activity.
7 months later she returned to PT with symptoms again. She was training for the Boulder Half Ironman again. She was advised to not run and consult with her neurosurgeon. Her symptoms pointed to a possible re-herniation.
She had her 2nd discectomy a few months later.
 One month after her 2nd discectomy, she emailed me stating changes in her bowel and bladder. I called her and told her to go to the ER. She had lumbar fusion at L5/S1. Goodbye Mr. Leaky Disc!
One month after her 2nd discectomy, she emailed me stating changes in her bowel and bladder. I called her and told her to go to the ER. She had lumbar fusion at L5/S1. Goodbye Mr. Leaky Disc!
She’s doing fine now with moderate activity. This is the actual picture of her sequestered disc…unbelievable!
Take Home Points
- Disc herniations are a common cause of back pain.
- Most disc herniations will heal on their own without surgical intervention.
- Core stability is imperative for a healthy back and to allow for optimal healing with a disc herniation.
- Go See a PT for Back Pain!
© 2018 and Beyond. ALL BLOG CONTENT at duncansportspt.com by Lori Duncan PT
ABOUT THE AUTHOR
 Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
References
Hahne AJ, Ford JJ, McMeeken JM. Conservative management of lumbar disc herniation with associated radiculopathy: a systematic review. Spine. 2010;35(11):E488-504.
Pourahmadi MR, Taghipour M, Takamjani IE, Sanjari MA, Mohseni-Bandpei MA, Keshtkar AA. Motor control exercise for symptomatic lumbar disc herniation: protocol for a systematic review and meta-analysis. BMJ Open. 2016;6(9):E012426.

Could you tell us please, how to distinguish Disc Herniation from Piriformis? Thank you!
Hi Cora,
Absolutely! In general, Piriformis Syndrome is annoying and painful, but it does not take your breath away. Disc herniations are usually more painful with transitions (sit to stand, rolling over in bed, getting out of the car) and they have the potential to take your breath away. Does that help?
12 years ago I had an x-ray that said I had a bit arthritis in my lower back. (I’m 70 y.o. now). Is that the same as “disk degeneration”? Can degeneration heal with proper exercise and posture or do you just prevent progression? I don’t have any back pain, but occasionally my back is a bit stiff in the morning for an hour or so. Recently I’ve also experienced a constant burning sensation in my left foot, and less often, an accompanying burning sensation in my buttocks (no pain just burning). Minimal in morning but worse in evening. Worse with laying on back or sitting on poorly supporting couch. No problem getting up and down or standing or walking or rolling over. I assumed it was piriformis, (doing figure 4 stretch on affected side makes foot tingle a bit and buttocks stretch is tender – i don’t do these -only as a test. No issue with stretch on unaffected side. I’ve also tried straight leg raise test with no issues). Is there a way to distinguish if burning is from arthritis/spine or piriformis? I’m starting doing these core exercises and your 2 glute exercises and see what happens. I’ll go to PT but with the wide range of approaches, I’d appreciate being prepared with your thoughts since your approach makes most sense to me compared to others. Sorry for the complicated questions. Thanks so much