Unexplained Body Pain: Muscle Atrophy and Fascia
The X-ray is normal. The MRI is negative. Every doctor visit leads you to more confusion and less answers as they say: “I’m not sure why you’re in pain.” So, they move you along. Not because they don’t care, but likely because they may not know. If the diagnostic tests, medical screens, blood work-up and imaging are all normal, why in the world are you in pain? From the doctor perspective, you look perfect. From the physical therapy perspective, it’s time to consider the bones, joints, ligaments and fascia and how they MOVE. Your pain may be muscle atrophy.
After 11+ years of treating patients, most unexplained body pain is usually muscle atrophy.
***Note: These cases of unexplained body pain have been cleared by the MD for anything significant or substantial.***
What is Muscle Atrophy?
Muscle atrophy is the loss of muscle bulk, size and girth because of poor activation. Clinically, it is known as muscle wasting. Atrophy is MUSCLE WEAKNESS to the Nth degree! Look at the picture below. Notice the difference in muscle size compared to the other. The left calf shows muscle atrophy.

Ok, so what caused this muscle atrophy or muscle de-activation?
Muscle atrophy can occur for several reasons, but the main categories are:
- Neurologic – the muscles receive less or no neurological signals from the brain or spinal cord region. This occurs from compression of the nerves at the spine, a neurological disease or from a significant neurological trauma such as spinal cord injury.
- Non-use – the muscles to do not receive a healthy nerve signal to do their job. Thus, they become unused. This occurs with pain, injury and movement compensation. This type of muscle atrophy will be the focus of this blog.
With pain or injury, most of us avoid movement in that area. And, further, the dysfunctional movement we use to “push through the pain” is muddy and unorganized. (Remember, movement in the body is a direct reflection of what is going on in the brain). After weeks, months and sometimes years of poor movement, the pain in your body starts knocking at your door:
“Please pay attention to me. I’m not well!”
Nerve Signals Move Muscles
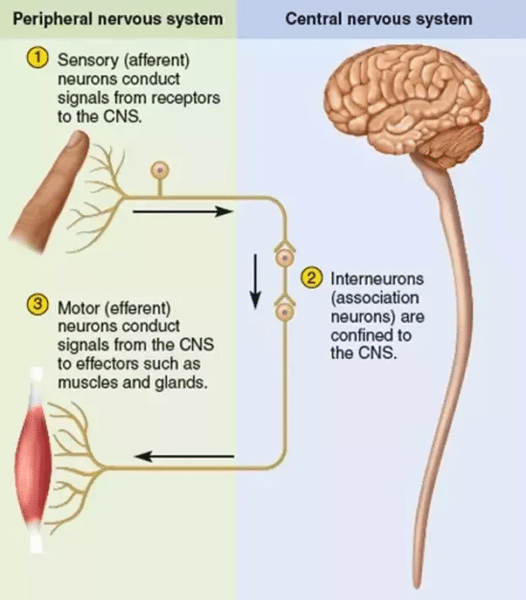
Image from Quora.com
Muscles and nerves communicate with each other. We have afferent nerves (nerves that take signals TO the Brain or CNS) and efferent nerves (nerves that bring signals TO the Body).
Here’s an example. Let’s say you stub your pinky toe on the corner of the wall. Now, that little pinky toe is really painful. A pain signal travels along the AFFERENT path TO the BRAIN and says:
“Hey there! I stubbed my toe down here. Kinda painful. Can you not walk on the outside of my foot. Thanks.”
Your brain answers and sends a message down the EFFERENT path TO the FOOT that says:
“Sure, I’ll have you hop on the other leg or walk on the inside of that foot so you don’t have to make contact with the ground where you stubbed the toe. I got you!”
Within seconds, you are limping or hopping and breathing in air through your teeth. You’re in pain! Thus, you avoid the outside of that foot until the pinky toe pain calms down.
Personal Story: When I was training for my Half Ironman in 2015, I stubbed my left pinky toe 3 times in one day. So ouchy! Running was not pretty that day. Luckily, I was smart enough to stop, come home and ice before I became a dysfunctional mess.
This is how it all begins. Pain occurs, we avoid using a specific area and a cascade of events follows. Muscle atrophy doesn’t happen after a day or two, but if the avoidance of that muscle or body region continues for months to years, then atrophy is the likely result. That makes sense, right? If you avoid using a muscle for long enough, the muscle tissue will decrease in size because of the lack of healthy nerve signals. Gradually, the muscle avoidance becomes muscle atrophy.
Why is Muscle Atrophy Painful?
 If a muscle is not getting healthy signals from the brain to move and activate, something will take over. For instance, at the hip area, the quadriceps, hamstrings and/or back like to take charge for the glute muscles. At the shoulder, the upper trapezius (big shoulder/neck muscle) loves to act as a scapular (shoulder blade) stabilizer. Neither of these muscle compensations end well. Pain and dysfunctional movement are the end result. And, the end result is a very painful myofascial syndrome (myo= muscle, fascia= connective tissue).
If a muscle is not getting healthy signals from the brain to move and activate, something will take over. For instance, at the hip area, the quadriceps, hamstrings and/or back like to take charge for the glute muscles. At the shoulder, the upper trapezius (big shoulder/neck muscle) loves to act as a scapular (shoulder blade) stabilizer. Neither of these muscle compensations end well. Pain and dysfunctional movement are the end result. And, the end result is a very painful myofascial syndrome (myo= muscle, fascia= connective tissue).
After months to years, the myofascial syndrome manifests into muscle atrophy pain. Now the weak and wasting muscles are actually tender to the touch. But, maybe it’s NOT the muscle that is painful. Likely, it’s the fascia elements around the muscle and its fibers. Fascia continues to be heavily researched. It’s characteristics, properties and capabilities are still being explored and quantified. However, we do know that fascia has nociceptors (pain receptors) that contribute to pain. So, if the glutes are lazy and they don’t want to work, yet the hip requires more stabilization than the hamstring and quad can deliver, what is your body left to use? Fascia. Connective Tissue. Yes, now your brain is really confused and unorganized and trying to use fascia for muscle activation.This is HIGHLY dysfunctional. And, painful.
How To Fix Muscle Atrophy from Non-Use
This is one of the easiest answers: MOVE THE MUSCLE. Activate it. Give it healthy signals. Re-organize your brain. One of the best ways to do this is with a physical therapist who understands the underlying cause of the initial pain (remember, that could have been a few years ago) and can help you re-activate your body with healthy tissue loading. Don’t waste your time with a non-medical provider. Seriously. Go See a Physical Therapist!
A Patient Story of Non-Use Muscle Atrophy
 In the Fall of 2017, a 45 year-old woman was referred to me with unexplained low back and hip pain. Two years before, she had fallen at work. She was highly compliant with PT, chiropractic care and massage through her Work Comp benefits. After 2 years of minimal improvement, the Workers Compensation System no longer believed her pain story and, thus, her case was settled out of court.
In the Fall of 2017, a 45 year-old woman was referred to me with unexplained low back and hip pain. Two years before, she had fallen at work. She was highly compliant with PT, chiropractic care and massage through her Work Comp benefits. After 2 years of minimal improvement, the Workers Compensation System no longer believed her pain story and, thus, her case was settled out of court.
Yet, at her initial evaluation this is what I wrote from her subjective statement:
” My MRI was negative for the hip and spine, but I only feel 65% of normal. I want to sit, work and walk without pain.”
She also stated a nagging “stretch” sensation in her left hip. After telling her history and beginning the evaluation, it was clear why she was in so much pain. For one, her left pelvic joint was significantly rotated, causing a “stretch” sensation to her hip. However, the most memorable finding was that every single tissue along her low back, left glutes and hamstrings were extremely tender to light touch. I was barely touching her, yet her pain was reflexive, reactive and high. Her connective tissue was trying to stabilize, move and do the work of the lazy glutes and leg muscles. Her muscle atrophy pain was the very end result of her pelvis getting rotated after the fall. Talk about a cascade of events!
Her 1st Treatment: neutral core activation, side glute lifts with a band for assistance, leg/pelvic dissocation. 4 exercises. That’s it.
After 7 treatments in 2 months, she stated she felt 90% of normal.
If you really listen to the patient, they will tell you exactly what is going on!
This blog post is dedicated to CM…a very special patient who inspired and encouraged me to write about this topic.
© 2018 and Beyond. ALL BLOG CONTENT at duncansportspt.com by Lori Duncan PT
***Update February 2019***
BLOG TALK PODCAST
Unexplained Body Pain: Muscle and Fascia
ABOUT THE AUTHOR
 Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
References
Willard FH, Vleeming A, Schuenk MD, Danneels L, Schlep R. The thoracolumbar fascia: anatomy, function, and clinical considerations. J Anat. 2012:221;507-536.

Lori has been my savior!
I have lived with unknown chronic pain for 2 1/2 years. I saw countless doctors and therapists for 2 1/2 years, had every image, test, scan and injection and no one had a clue.
I would never give up though and one night last June I found Duncan Sports Therapy and the rest is history. Even though I live in Texas Lori agreed to try Face time sessions, (my husband played cameraman) and I began to see improvement after the first session. I am 7 months in, I still have a ways to go but I am 85% improved. It is hard work and painful at times but sooooo worth it! My end goal is to be able to squat to the floor again!
I cannot find words to thank Lori for what she has done for me. I will be forever indebted.
Thanks Lori for all your great posts. Wish I could come see you.
Hi Jen,
Thanks for your kind comment and reading the posts. Glad they are helpful.
The whole 1st section sounded like what is going on with my husband. Muscle atrophy in his calf, but he has no feeling in it. Nerve tests, spinal taps, blood work, 15 different xrays, 5 MRIs…no explanation at all. We have no answers and no way of “fixing it”.
Hi Tracey,
Well, tell him to start working on finding those muscles. I assume he’s had an mRI on his entire spine (I had one patient with undiagnosed weakness and no one had taken a picture of her thoracic spine. She had a tumor pressing on her spinal cord. She’s fine, but no one had thought to look). If he’s clear, then he can feel better. The body has so much potential to heal itself.
Hello Lori,
My name is Jason and I actually am writing on behalf of my Dad. He has had severe back pain mainly lower for the last several years. He has been to all kinds of doctors and had many tests but no solution found. Now to let you know 10 years ago they found a tumor on his spine and it has been monitored with no growth in size. Within the last year he notice his one calf muscle that is smaller than his other one. He might average one day a month with little to know pain. Any ideas?
Hi Jason,
Hmm…if his calf is decreasing in size one of two things is likely going on. 1. That tumor is actually causing neurological damage and his calf receives less input to fire the muscles. 2. The pain in his body is keeping him from avoidance of using that calf. Are you sure that tumor isn’t compressing his spinal cord? It’s not normal to be in that kind of pain. Have you had a recent MRI of his thoracic and lumbar spine?
Thanks for the response. I got more info that might add some info on the timeline of everything. 12 years ago he fell off our roof which was about 14ft in the air. When he fell he landed on both feet saying the right side took a little more impact. No pain till two years later in which he had a MRI. They found the tumor at that point. They attributed his pain to the tumor and said they would continue to monitor the tumor for growth. He has had the tumor MRI several times most recently a couple of months ago with no growth as it has stayed the same. The last MRI revealed what one doctor saw as a narrowing spot of the spine and a bunch of arthritis in his back. The pain has been consistently in the lower back and I stand corrected that he says he averages one day a year pain free. Other pain he has is shoulder pain and leg pains in the knees. Shoulder pain tends to be muscle pain and has been consistent for the last three months. Both knees hurts ever so often and he has weakness in both legs every now and then. It all occurs at different times. We noticed the right leg muscles was smaller in mass than the left leg about six months ago, this includes the thigh, calf, and right glute. The one doctor that found the narrowing spinal canal suggested a series of epidural shots in the spine. The first he received had him pain free for 3 full days and then the pain returned. He had his second last week and it was given a little lower than the first and it lasted pain free for one day. His hopes were really high that the shots were the answer however those hopes seemed to have lessened. I know this is a lot but I wanted you to have everything that could be related. Your advice would be valued. Thank you.
Hi Jason,
Well, gosh that is a big history. Where do you all live? Maybe I can refer you to someone. There are so many questions to ask and have answered to give great advice. I wish I had a simple thought for you, but too many things to tease out. I do over online consults if you are interested. Let me know!
Good information, but I’m wondering if atrophied muscle due to spinal injuries can be reversed??
Hi Darin,
It depends on the spinal injury. If it is complete spinal cord injury, then no. If it is incomplete spinal cord injury, possibly. If it is a spinal injury from stenosis, disc herniation or other pressure on the nerve root, then there is almost always potential. It just take someone skilled to tap into that potential. Does this answer your question?
I had a surgery on my left leg as a baby and after 24 years I am feeling the pain again..the place where the mark is on the leg is thinning gradually… and I am in pain for the past one year over it….. how can I deal with this problem
I had a surgery on my left leg as a baby and after 24 years I am feeling the pain again..the place where the mark is on the left leg is thinning gradually… and I am in pain for the past one year ….. how can I deal with this problem
Hi,
You need to find exercises to activate those muscles with minimal to no pain (ideal). That might start as some isometrics (quad sets, glute squeezes, hamstrings). The worst thing you can do is not move.
Hi Lori,
I had Guillain Barre Syndrome almost 30 years ago, have a lot of residuals and walk with an assistive device (AFO for foot drop and a cane). For years, I walked without the AFO and initially believed that the back pain was due to overcompensating. My back muscles are extremely tight and I often have spasms. Is there a specific test or imaging to determine muscle atrophy in my back? As this is due to residual nerve damage, can it be reversed? Any assistance you can provide is greatly appreciated.
Thank you
Hi Tina,
There really is no image to test for atrophy, thus why it does “missed” so often. But, if you find a good PT they should be able to determine which tissue is atrophied. It’s very obvious to my hands or how the body moves. I know you had GBS, but I always tell my patients that there is usually more potential for the body to heal and perform better if it loaded correctly. Especially if the atrophy is more from non-use than true neurological damage. I’d find a good PT and find the potential of what your body can do. Possibly look for a Pilates-based PT. Hope that helps!
Hello Lori,
Thank you so much for your response! I’d never heard of Pilates PT until I came across your post.
I was able to locate Pilates PT a facility near my home and will reach out to them.
Thanks again for providing this valuable information.
Take care,
Tina
Can you help one whose calf was ravaged by polio 60 years ago?
After breaking tibia, fibula and pilon fractures, an external fixation then 2nd surgery removal and insertion of 2 large plates and 20screws then a 3rd surgery, a tendon lengthening in 3 places. Been diagnosed with Rrps type 1 , plantar fasciitis and mild Osteoarthritis now pt says they can’t do anything more because of painful Crps and muscle atrophy. One dr suggest nerve blockers &spinal injections I am just tired of hurting, have not been able to bear weight in over a year, after recovering from 2nd surgery once allowed to bear as tolerated I begat multiple muscle hernias near the surgical site.