Plantar Fasciitis
Although it may feel like it at the time, this is not a death sentence for your foot. Wow, that heel pain is intense. It travels to your arch. You dread waking up in the morning to experience those first few steps. Walking barefoot becomes almost unbearable. Will you ever run, let alone walk, without pain? For most of my patients, I confidently say: YES.
I will preface this post by stating that plantar fasciitis continues to be an ever-evolving diagnosis with many opinions on the best way to treat it. There are many factors to consider (foot anatomy, gait mechanics, soft tissue stresses and activity level), but it seems to strike anyone: thin, overweight, running shoes, flip-flops, young, old, male, female, etc…you get the point. In my opinion, the common denominator for everyone is their gait mechanics, including the windlass mechanism. (If I lost you on that last sentence, keep reading. I promise it will make sense in a few minutes.)
Gait is a highly complex function that we take for granted…until we have pain. Gait begins at the trunk, pelvis and hip complex and continues down to the knee, ankle and foot. For simplicity and educational purposes, this blog will take a simplified look at the mechanics of the foot to better understand plantar fasciitis.
Let’s take a step back (ha, get it…step back!) from gait and consider the common approach to treating this painful diagnosis.
Here are the top interventions recommended by health care providers and the all-mighty internet :
- Stretch the calf muscles
- Night splints
- Orthotics
- Toe stretches
- Toe crunches
The next level of intervention:
- Extracorporeal Shock Wave Therapy
- Cortisone Shots (ouch!)
If conservative treatment fails (less than 5% of individuals with plantar fasciitis):
- Surgery
NOTE: None of the interventions above mention gait.
What is the plantar fascia and what does it do?
The plantar fascia, or plantar aponeurosis, is a thick, elastic band that expands length-wise from the calcaneus (heel bone) to the metatarsal heads and phalanges (toes). Like other fascia in the body, it stores energy and allows for efficient propulsion (walking, running or jumping).
What is the windlass mechanism?
A windlass is an apparatus used to move heavy objects. Considering the body, the plantar fascia is the apparatus that winds up to move the foot, thus body (the heavy object), through space.
The windlass mechanism is a position of the foot that occurs with normal gait mechanics. It was originally described by John Hicks in 1954. He described the foot as a truss (triangular unit) with the plantar fascia acting as a tie rod (a structural unit meant to hold tension).
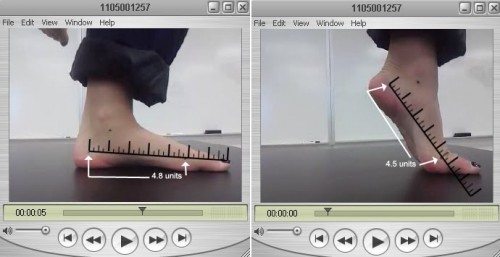
When our heel contacts the ground, the foot quickly moves to pronation to increase foot mobility and allow the foot to respond to the terrain beneath it. This foot position stresses and stretches the plantar fascia in preparation for the next phase.
Toward the end of stance phase, the heel lifts off the ground, the toes extend (dorsiflex), and the foot moves to supination, causing the plantar fascia to “wind up,” shorten and raise the arch. This creates the truss and is named the windlass mechanism. This shortened position creates “rigidity” or stiffness to the foot and allows the foot to act as a rigid lever to move the body through space.
Slide one shows the pronated foot. Slide two shows the supinated foot. Note the difference in plantar fascia length.
What causes plantar fasciitis?
That is the BIG question and the professional duty of the physical therapist to figure out. For some it is bony anatomy, for others it is soft tissue irritation after a change of shoe wear. For most patients, it is the imbalance between pronation and supination that results in irritation and inflammation of the plantar fascia. That makes sense right? That if the tissue is not allowed to move through its natural range of motion it could become a little ticked off?
Other common scapegoats of plantar fasciitis:
- Pronated foot: we now know from research this is not always an indicator
- Supinated foot: same as above
- Poor or change of shoe wear: is it the shoe or did the new shoe change the gait mechanics?
- Running or standing surface (concrete): Yes, concrete has absolutely no ability to help with ground force absorption
- Overweight: the plantar fascia does absorb the body weight. However, if you have the muscle stability to support the weight, is this as much of a factor?
The following are the main culprits I have found in my clinical practice.
- Faulty gait mechanics
- Lack of foot intrinsic strength
- Lack of hip and ankle stability
- Restricted plantar fascia mobility
- Decreased calf and FHL (big toe flexor) mobility and length
All of the above are supported in research, except #2. I cannot find one research article that supports the training of the foot intrinsics (interossei, lumbricals) as an intervention for plantar fasciitis. These are the stability muscles of our foot. And, remember, we need stability for efficient mobility.
Blog Activity
Find your foot intrinsics
- Sit at the edge of your chair and hold your foot out in front of you.
- Spread your toes away from each other (just like you would spread your fingers in your hand)
- Theoretically, your toes should spread away from each other.
- For most, this takes some practice to master.
Final note: toe crunches are commonly prescribed for plantar fasciitis, but this exercise is highly ineffective for this diagnosis. Most of us curl our toes for stability because of the lack of intrinsic strength. This exercise does not isolate the true intrinsics of the foot and can further exacerbate symptoms in an already toe curling walker.
There is a reason your foot has plantar fasciitis. Get to the root of the issue, and you should be able to walk sooner than later without pain.
© 2014 and Beyond. ALL BLOG CONTENT at duncansportspt.com by Lori Duncan PT
ABOUT THE AUTHOR
 Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.
Lori Duncan, DPT, MTC, CPT is a respected Physical Therapist, Manual Therapist and Pilates instructor in Lafayette, CO. Lori is passionate about preventive physical therapy and education and is a nationally recognized presenter. She can be reached at [email protected]. You can also follow Duncan Sports Therapy + Wellness on Facebook & Instagram for more free tips and information.


Hi,
It is funny how you mention spreading your toes, I used to be able to do this really well and freak out my friends but I have found that now I have fasciitis I am unable to do this.
I cured one foot by curling my toes and allowing my foot to cramp several times. I have no idea how that fixed it, but it worked. My other foot is still a problem and I also have knee, hamstring and back pain on that side so it may need a more complex solution.
Keep up the good work, love the site
Stuart
Hi Stuart,
Thanks for reading my site! I appreciate the feedback. Interesting about the toe curling fixing your foot. Yes, sounds like you may have more going on the one side. Back to foot pain is not normal. Maybe get that checked out!
Hi Lori! Thanks for the great article. I struggle with right heel pain and have been xrayed which shows no heel spur. I cannot spread my toes as you show above. I have tried strengthening with toe raises which I do believe has helped. Also using a foam roller on my calves has helped. Do you have any other suggestions for me?
Also, I was found to have a more prominent fascia on the right side where my pain is. Orthotics have not really helpes with the exception of the cheaper ones found in the stores. The hard ones from the podiatrist made it worse.
Also, I was found to have a more prominent fascia on the right side where my pain is. Orthotics have not really helpes with the exception of the cheaper ones found in the stores. The hard ones from the podiatrist made it worse.
Hi Jennifer,
Thanks for reading! Work on spreading those toes for good foot intrinsics. And, your calf raises (I assume that’s what you mean by toe raises) are a good thing, but do them eccentrically. Meaning, go up on 1 count and then slowly lower down on 3-4 counts. There is more and more research about how that can be effective for plantar fascia. I’m not a huge fan of foam rolling the calf muscles as it can be a little invasive to that area. If you feel you are mild/gentle, should be ok. Most people apply WAY too much pressure and the muscle can “fight” back and never relax. And, hard orthotics are terrible. There are some great orthotics out there, but it should never be a hard plastic. And, make sure you are walking through that foot as much as possible, especially in your home where you have some soft carpet. Hope that helps!